President Biden’s Inflation Reduction Act cracks down on Big Pharma price gouging, saving some seniors thousands of dollars per dose of medication. Meanwhile, Congressional Republicans push for giveaways to drug industry

President Biden visited the National Institutes of Health Clinical Center in Washington, D.C. to announce that dozens of pharmaceutical companies will be required to pay rebates to Medicare for outrageous price hikes on prescription drugs that over 750,000 seniors take per year. For the last quarter of 2023, 48 Medicare Part B drugs raised their prices faster than inflation, and some drug companies raised prices of certain medications faster than inflation for every quarter over the last year. President Biden’s Inflation Reduction Act cracks down on this exorbitant price gouging, requiring these companies to pay rebates back to Medicare, saving seniors who take these drugs between $1 and $2,786 per dose on their medication.
President Biden vowed to lower prescription drug costs for seniors and families – and he is delivering on that promise. His Inflation Reduction Act finally allows Medicare to directly negotiate lower prescription drug prices, capped the cost of insulin for Medicare beneficiaries at $35, made recommended adult vaccines free, requires drug companies to pay rebates if they raise prices faster than the rate of inflation, and locked in savings of $800 per year on health insurance for nearly 15 million Americans. While Republicans in Congress fight tooth and nail to repeal the Inflation Reduction Act and put money back in the pockets of Big Pharma, President Biden won’t back down from the fight to lower costs for hardworking Americans and make sure every family has access to affordable health care.
The Biden-Harris Administration announced:
- The Department of Health and Human Services (HHS) announced a new list of 48 Medicare Part B drugs that raised their prices faster than inflation, and may be subject to inflation rebates in the first quarter of 2024 as a result of the Inflation Reduction Act. President Biden’s prescription drug law cracks down on price gouging from Big Pharma, requiring companies to pay back Medicare if they raise prices on seniors at a higher rate than inflation. Starting in January, some Medicare beneficiaries who take these 48 prescription drugs – including drugs used to treat cancer and fight infections – will have lower coinsurance than what they would have paid otherwise, and their out-of-pocket costs may decrease by $1 to as much as $2,786 per average dose.
Over the last four quarters, 64 drugs in total had prices that increased faster than inflation and may be subject to inflation rebates because of the Inflation Reduction Act. Some drugs, such as Signifor, used to treat an endocrine disorder, raised prices faster than inflation every quarter since the Inflation Reduction Act’s inflation rebate provision went into effect. Some Medicare beneficiaries who take Signifor could save $311 per monthly dose starting January because of the law.
The Administration is focused on making sure medications developed with taxpayer funds are available to Americans at reasonable prices. On average, Americans pay 2 to 3 times more than consumers in other developed countries for prescription drugs. Last week, the Administration announced a proposal to put drug companies on notice if products developed using federal funds are not made available to the public on reasonable terms, including based on price. The proposal would promote the federal government’s ability to license a patent — such as those used to create life-saving drugs — to a competitor with the goal of increasing competition and bringing costs down for families.
Building off last week’s announcement, today HHS announced that the Administration for Strategic Preparedness and Response (ASPR) is making fair pricing a standard part of contract negotiations for medical products developed or purchased as part of its commitment to obtain best value for the US taxpayer. In September 2023, ASPR finalized a Project NextGen contract agreement for a potentially life-saving COVID-19 treatment being developed by Regeneron stating if the product is commercialized, its list price in the United States will be equal to or less than its retail price in comparable global markets. Since then, ASPR has also included similar language in recent agreements with CastleVax, Codagenix and Gritstone Bio, developers of the first three vaccines selected for development within Project NextGen. These clauses will be in effect if and when a company’s candidate vaccine is selected to move into ASPR-supported Phase 2b trials to evaluate clinical safety and efficacy.These actions are the result of a successful and collaborative approach by ASPR and its industry partners and show HHS’s commitment to keep Americans from paying unfair prices for the care they need.
- HHS is releasing new data on the ten drugs selected for Medicare Drug Price Negotiation. For Medicare enrollees who take these drugs, their out-of-pocket spending on the 10 drugs selected for negotiation represents, on average, over half of their total Part D out-of-pocket spending. The report shows that total Medicare spending on the 10 drugs more than doubled from 2018 to 2022 – a rate that was 3 times faster than all Part D drugs over the same period. The report also shows that 7 of the 10 drugs selected received direct at least one form of federal support towards their drug development or utilized a federal-funded invention for their development.
After decades and hundreds of billions of dollars spent by Big Pharma to block Medicare from directly negotiating lower prescription drug prices for people with Medicare, President Biden’s Inflation Reduction Act finally got it done. In total in 2022, Medicare Part D beneficiaries paid $3.4 billion in out of pocket costs for the 10 drugs selected for negotiation, and some paid over $6,000 per year for just one of the drugs on the list. Negotiated prices will go into effect for seniors in 2026.
Today’s announcements build off the actions the Administration has already taken to lower prescription drug costs for millions of seniors and families because of President Biden’s Inflation Reduction Act. In 2023 alone:
- The Inflation Reduction Act saved nearly 15 million Americans an average of $800 in 2023 because of health insurance savings the law locked in.
- The Inflation Reduction Act capped the cost of insulin at $35 per covered insulin product for Medicare beneficiaries, saving an estimated 1.5 million seniors on Medicare $500 on average in 2023 on insulin costs.
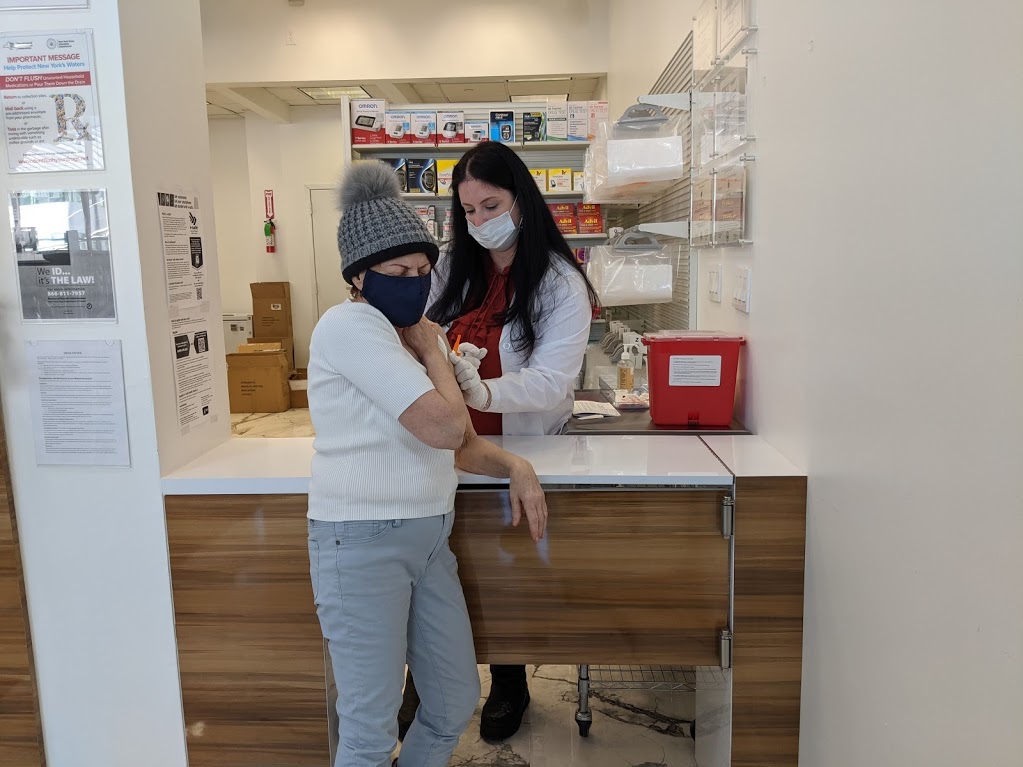
- The Inflation Reduction Act made recommended vaccines – like the shingles vaccine – free for the 50.5 million seniors with Medicare Part D, and made recommended, approved adult vaccines free for all adults in the Children’s Health Insurance Program, and nearly all full-benefit adults enrolled in traditional Medicaid. Seniors on Medicare who received a Part D vaccine saved an average of $70 on vaccines in 2023.
- The Inflation Reduction Act saved many seniors on Medicare as much as $618 per average dose on 47 prescription drugs in 2023 because of the law’s provision requiring drug companies to pay rebates on certain drugs if they raise prices for those drugs faster than the rate of inflation. Starting in 2024, some seniors who take 48 prescription drugs could see savings of as much as $2,786 per average dose because those 48 drugs raised their prices faster than inflation in the last quarter of 2023.
- The Inflation Reduction Act capped the cost of insulin at $35 per covered insulin product for Medicare beneficiaries, saving an estimated 1.5 million seniors on Medicare $500 on average in 2023 on insulin costs.
In the coming months and years, the Inflation Reduction Act will continue to deliver cost-savings to millions of Americans, including:
- In 2024, Part D enrollees will no longer pay 5% co-insurance when they reach the catastrophic phase of their benefit – meaning that some beneficiaries’ prescription drug costs will be capped at about $3,500 next year.
- When the $2,000 out-of-pocket cap on prescription drugs applies in 2025, nearly 19 million seniors and other beneficiaries are projected to save $400 per year on prescription drugs. 1.9 million enrollees with the highest drug costs will save an average of $2,500 per year because of this provision of the Inflation Reduction Act.
- When the $2,000 out-of-pocket cap on prescription drugs applies in 2025, nearly 19 million seniors and other beneficiaries are projected to save $400 per year on prescription drugs. 1.9 million enrollees with the highest drug costs will save an average of $2,500 per year because of this provision of the Inflation Reduction Act.
Millions of seniors could save money when negotiated prices of the first group of drugs selected for the Inflation Reduction Act’s Medicare Price Negotiation program are scheduled to go into effect in 2026. In 2022, seniors spent $3.4 billion in out-of-pocket costs on the first ten drugs selected for negotiation – used to treat common conditions like diabetes, Crohn’s disease, arthritis, blood clots and more. A report released last week shows that had the Medicare price negotiation program been in effect in 2021, Part D out of pocket costs would have declined 23% for people taking the ten costliest drugs at the time.
The Congressional Republican Agenda on Prescription Drugs: Giveaways to Big Pharma and Higher Costs for Seniors and Families
While President Biden has taken historic action to reduce prescription drug costs for seniors and for working-age people who get health insurance through their jobs, Congressional Republicans are actively fighting to roll back the reforms the President signed into law and to keep Big Pharma’s taxes low.
Congressional Republicans’ agenda for Big Pharma giveaways includes:
Repealing prescription drug inflation rebates. The Inflation Reduction Act (IRA) cuts costs for Medicare and seniors by requiring pharmaceutical companies to pay a rebate to Medicare if they increase prices faster than inflation. Dozens of Republicans have signed onto legislation that would revoke the rebate requirement.
By 2031, repealing this provision would:
- Cost seniors $5 billion per year.
- Increase federal deficits by $7 billion per year.
- Give away over $10 billion per year to pharmaceutical companies.
Taking away Medicare’s ability to negotiate prescription drug prices. The IRA finally gave Medicare the authority to directly negotiate with drug companies on the high prices they charge for prescription drugs. Republican Chairs and Ranking Members of the committees with jurisdiction over Medicare have publicly committed to repealing this authority, which would allow Big Pharma to go back to charging seniors exorbitant prices for life-saving drugs.
By 2031, repealing this provision would:
- Cost seniors $7 billion per year.
- Increase federal deficits by $14 billion per year.
- Give away over $20 billion to pharmaceutical companies per year.
Opposing caps on insulin prices. Monthly insulin costs for Medicare beneficiaries are now capped at $35—providing certainty and critical cost savings for seniors who in some cases were paying as much as $400 for a month’s supply of insulin. The Republican Study Committee budget, as well as the House Budget Committee-passed budget plan, propose to repeal this and other IRA drug price reforms.
Repealing this provision would mean the 1.5 million Medicare beneficiaries who use insulin could see their annual costs rise by an average of $500.
Protecting Big Pharma’s ability to avoid paying taxes. President Biden negotiated a historic agreement with over 130 countries that would enable the U.S. and its partners to ensure Big Pharma and other multinationals pay at least a minimum tax rate and has proposed that the U.S. implement that agreement with a 21% minimum tax rate on multinationals. Congressional Republicans are not only blocking the U.S. from implementing the global minimum tax agreement and vowing to never raise taxes on Big Pharma and other multinationals by implementing it, they also traveled to Europe this summer to try to persuade other countries to withdraw from the global agreement and keep taxes low for Big Pharma and other multinationals.
Blocking implementation of the President’s international tax reform proposals means:
- Protecting a system in which Big Pharma can lower its taxes to under 12% by shifting profits offshore.
The U.S. would lose out on hundreds of billions in savings from adopting the President’s proposals to implement the international agreement. Based on a PhRMA-funded analysis, nearly $100 billion of the savings – or almost one-fifth of the total revenue – from implementing the President’s 21% minimum tax proposal would come from cracking down on pharmaceutical industry tax avoidance