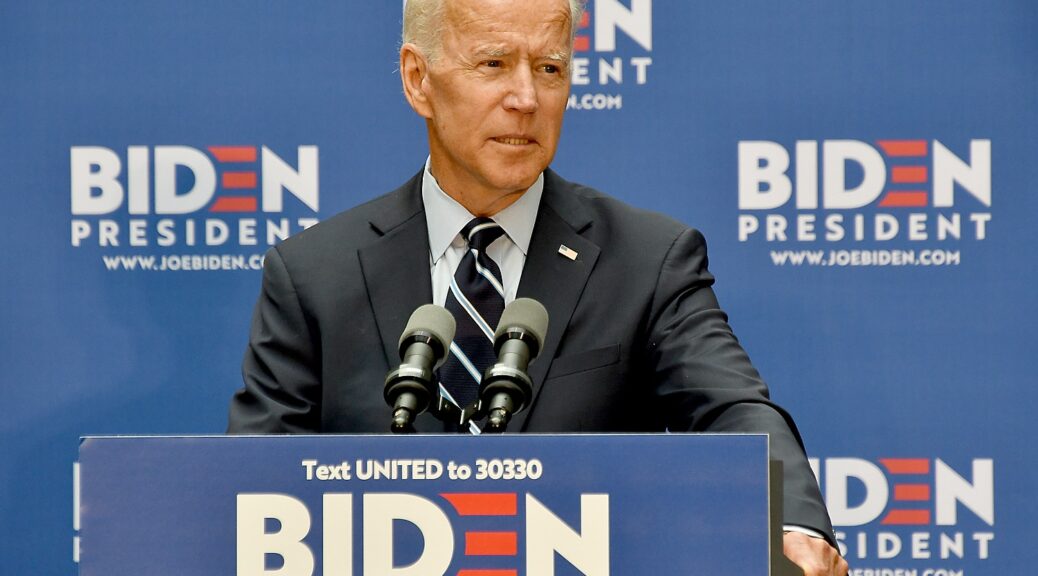
The White House provided this fact sheet detailing actions President Biden has taken, and new actions he is taking to lower prescription drug and health care costs, expand access to health care and protect consumers, even as Republicans voted against giving Medicare the ability to negotiate drug prices and their presumed presidential nominee, Trump, is renewing calls to repeal the Affordable Care Act (Obamacare), which now has enabled a record 21 million to obtain health insurance, 9 million more than when Biden took office, and as he moves to negotiate for a $2000 cap on out-of-pocket prescription drug costs for all, not just Medicare recipients and expand the number of drug prices being negotiated from 10 to as many as 50 a year. –Karen Rubin, [email protected]
President Biden believes that health care is a right, not a privilege, and since day one, he has delivered health care to millions more Americans while also lowering health care costs. The President continues to build on, strengthen, and protect Medicare, Medicaid, and the Affordable Care Act, signing laws such as the American Rescue Plan Act and the Inflation Reduction Act to lower prescription drug costs and health insurance premiums. Thanks to the President’s efforts, more Americans have health insurance than under any other President, and are better protected against surprise medical bills and junk fees. Seniors are already seeing lower prescription drug prices with insulin capped at $35, free vaccines, and out-of-pocket costs for prescription drugs capped at $2,000 starting in 2025. And the Administration is well on its way to lower the cost of range of drugs as Medicare negotiates over the prices of prescription drugs for the first time ever. The Biden-Harris Administration has also taken steps to make sure consumers aren’t scammed by junk insurance and have better access to mental health care.
However, the President is not just resting on these accomplishments. He’s fighting to deliver even lower costs and better health care to Americans. That’s why the Biden-Harris Administration is acting to lower prescription drug costs, keep health insurance premiums low, expand access to health care, especially mental health care coverage, and continue to protect Americans from getting ripped off.
Taking on Big Pharma to Deliver Lower Prescription Drug Costs for Seniors and Families
After decades of opposition, President Biden enacted a law that finally takes on Big Pharma and gives Medicare the power to negotiate drug prices. President Biden’s Inflation Reduction Act will save millions of seniors money on some of the costliest prescription drugs on the market. Meanwhile, Big Pharma also executed over $135 billion in mergers and acquisitions in 2023 alone, while passing the cost to consumers. And eight of the 10 drugs selected for this year’s negotiation program raised their prices in 2024 – after all 10 drugs were already priced three to eight times higher in the United States than in other countries. President Biden knows how the Inflation Reduction Act is delivering for American families, and his Administration will continue the fight to lower health care costs for more Americans.
- Announcing that Manufacturers of 10 Drugs Remain at the Negotiating Table. Last month, for the first time in history, Medicare has made offers on the fair price for 10 of the most widely used and expensive drugs. Medicare is no longer taking whatever price for these drugs that the pharmaceutical companies demand. This week CMS announced that manufacturers for all 10 selected drugs are participating in drug price negotiation, with all manufacturers having submitted counteroffers and negotiations continuing. Later this year, new, negotiated prices for the first 10 prescription drugs selected for the negotiation program will be announced.
- Let Medicare Negotiate Drug Prices for at least 50 Drugs Every Year. Medicare should not be limited to negotiating just 20 drugs per year. Instead, the President is proposing that Medicare be able to negotiate prices for the major drugs that seniors rely on, like those used for treating heart disease, cancer, and diabetes. The Budget cuts federal spending by $200 billion increasing the number of drugs Medicare can select for negotiation and bringing more drugs into the negotiation process sooner, and other reforms.
- Expand Cap on Out-of-Pocket Prescription Drug Costs. When the $2,000 out-of-pocket cap on prescription drugs applies in Medicare in 2025, nearly 19 million seniors and other beneficiaries are projected to save $400 per year on prescription drugs. The President is calling on Congress to expand the $2,000 out-of-pocket cap to all private insurance so that all Americans have the peace of mind that comes with knowing that they won’t have to choose between filling their prescription or putting food on the table.
- Capping Medicare Cost-Sharing at $2 for Common Generic Drugs. Medicare will be launching a new model to limit Medicare Part D cost-sharing for certain generic drugs to $2. As Medicare prepares to launch the model, today HHS published a list of dozens of generic drugs for the model, including drugs like statins to treat high cholesterol, beta-blockers for high blood pressure, and platelet inhibitors to prevent blood clots. In his budget, the President is calling on Congress to limit Medicare cost-sharing to $2 for high-value generic drugs for all Medicare plans.
- Access to Cell & Gene Therapies. In January, HHS announced that sickle cell disease will be the first focus of the Cell and Gene Therapy (CGT) Access Model. Under this model, CMS will negotiate with manufacturers on behalf of state Medicaid programs to increase affordable access to potentially lifesaving and life-changing treatment, and lower health care costs for some of the nation’s most vulnerable populations. Today, CMS is releasing the Request for Applications for drug manufacturers of cell and gene therapies to participate in the model.
- Expand the IRA’s Requirement that Drug Companies Pay Rebates When They Increase Prices Faster than Inflation. Thanks to the IRA, drug manufacturers must now pay rebates to Medicare if their price increases for certain drugs exceed inflation. The President is calling on Congress to require those rebates for commercial drug sales, as well as sales to Medicare. That will save the federal government billions of dollars, further curb prescription drug price inflation, and reduce health insurance premiums for people with private health insurance coverage.
Putting High-Quality Health Care Within Reach
Today, more Americans have health insurance than under any President. The President’s efforts to lower health insurance premiums have led to record-breaking enrollment in the Affordable Care Act’s Marketplaces, with over 21 million people signing up for coverage – 9 million more than when the President took office. The Biden-Harris Administration isn’t stopping there and is building on this incredible success by:
- Keeping Health Insurance Premiums Low. Thanks to the President’s American Rescue Plan and Inflation Reduction Act, millions of Americans are saving on average $800 a year on premiums. The Biden-Harris Administration is committed to keeping health insurance premiums low, giving families more breathing room and the peace of mind that health insurance brings. To do that, the President is calling on Congress to make the expanded premium tax credits that the Inflation Reduction Act extended permanent. Without Congressional action, millions of Americans will see their health insurance premiums spike by hundreds or thousands of dollars starting in the fall of 2025.
- Closing the Medicaid Coverage Gap. The President continues to call on Congress to provide Medicaid-like coverage to people in the 10 states that have not adopted Medicaid expansion as well as keeping Medicaid expansion enrollees covered.
- Keeping Kids Covered. Investing in our nation’s children is a top priority for the President. Research shows that when children have health insurance, they thrive: they’re healthier, they do better in school, and are more likely to succeed in adulthood. Keeping children covered is the right thing to do, which is why the President wants to make sure that children can never lose coverage due to red tape from birth until they turn age 6, and that families only have to submit Medicaid paperwork once every three years.
- Closing Research Gaps in Women’s Health Research. In November 2023, the President and the First Lady launched the first-ever White House Initiative on Women’s Health Research to fundamentally change how our nation approaches and funds women’s health research. Women make up more than half the population but have been understudied and underrepresented in health research for far too long. As part of the initiative, the President during the State of the Union will call on Congress to make bold, transformational investments in women’s health research.
- Making Home Care More Available. Thanks to the American Rescue Plan, President Biden delivered $37 billion to all states to expand access to home care and improve the quality of caregiving jobs. The Biden-Harris Administration is taking steps to improve the quality of Medicaid home care services and to make sure home care workers get a bigger share of Medicaid payments for these critical services. The President remains committed to further improving and expanding Medicaid home care services, and is calling on Congress to do their part to allow the hundreds of thousands of older adults and individuals with disabilities on Medicaid home care waiting list to remain in their homes and stay active in their communities while continuing to improve the quality of jobs for caregivers.
- Ensuring Access to Mental Health Care. Ensuring robust access to mental health care has been a bipartisan priority for almost 15 years, including the enactment of mental health parity requirements which require health plans to cover mental health care benefits at the same levels as physical health care benefits. Yet today, too many Americans still struggle to find and afford the care they need. The President is committed to tackling the mental health crisis in this country, which means making health plans do their part and providing agencies with the needed support to make sure they’re doing so. The Biden-Harris Administration is working to finalize the mental health parity rule, which would close existing loopholes as well as ensure health plans evaluate access to mental health care in their networks, and make changes if it’s found to be inadequate. In addition, the President is calling on Congress to further increase access to mental health care by expanding coverage in Medicare and private insurance, applying the mental health parity requirements to Medicare beneficiaries, and extending Medicare incentive programs to address mental health provider shortages.
Cracking Down on Junk Insurance, Surprise Bills and Fees, and Confusing Health Care Pricing
Nothing infuriates the President more than seeing Americans get ripped off. That’s why the Biden-Harris Administration has prioritized implementing surprise billing protections, preventing 1 million Americans from receiving surprise medical bills every single month. The President has also taken steps to prevent Americans from being ripped off by junk insurance that preys on vulnerable citizens by closing loopholes to ensure consumers know what they’re buying and can get the health coverage that best meets their needs. But more can be done to protect consumers, which is why the President intends to:
- Prevent More Surprise Medical Bills. Today, Americans are protected from receiving medical bills for most emergency care and air ambulance services as well as when consumers didn’t know they were getting care from an out-of-network provider despite doing their homework and going to an in-network facility for treatment. The President wants to further protect consumers by applying surprise billing protections to ground ambulance providers. The last thing people should worry about during an emergency is an unexpected bill for their ambulance ride.
- Crack Down on Junk Insurance. Last year, the Biden-Harris Administration proposed a monumental rule to help millions of Americans access high-quality, affordable health insurance and protect consumers from being discriminated against because of pre-existing conditions. Making sure Americans aren’t scammed into low-quality coverage, and charged more or denied life-saving care is a key priority for the Administration, which is why we are working to finalize proposed rules that limit the availability of junk insurance.
Honoring America’s Commitment to Seniors
The President has always believed that Medicare and Social Security are a promise—a rock-solid guarantee generations of Americans have counted on to be able to retire with dignity and security. The President will reject any efforts to cut the Medicare or Social Security benefits that seniors and people with disabilities have earned and paid into their entire working lives. The Budget honors that ironclad commitment—not only by rejecting benefit cuts, but by embracing reforms and investments that will protect and strengthen both programs. The President is committed to working with Congress to ensure Medicare and Social Security remain strong for their beneficiaries, now and in the future.
- Securing Medicare. In his budget, the President is calling on Congress to ensure that high-income individuals contribute their fair share to Medicare and directs revenue from the Net Investment Income Tax into the HI trust fund as was originally intended. In addition, the President has proposed to direct savings from further lowering drug costs into the Medicare trust fund. If Congress were to heed the President’s call and enact these reforms, it would substantially extend solvency for the Medicare HI Trust Fund, guaranteeing seniors the benefits they have been promised.
- Protects Seniors’ Health and Dignity. As President Biden pledged to do two years ago in the State of the Union, the Biden-Harris Administration is “set[ting] higher standards for nursing homes and make sure your loved ones get the care they deserve and that they expect.” The nursing home industry receives billions of dollars of taxpayer funding each year, but for too long, many facilities have not had the staff required to give residents safe, high-quality care. That is changing. HHS has proposed a new rule establishing a federal floor for nursing home staffing, so that owners cannot cut staffing to unsafe levels simply to turn a profit. This includes a proposal for every facility to have a Registered Nurse on site 24/7, in addition to minimum number of registered nurses and nurse aides to assist with care. Earlier this year, HHS also finalized a rule to increase transparency in nursing home ownership, making it easier for residents and their loved ones to hold facilities accountable. The final rule was just submitted to the Office of Management and Budget for review
Strong Record on Expanding and Strengthening Health Care Nationwide
The President’s new actions are all in addition to an already impressive track record on fighting for the health care of Americans across the nation. Over the last three years, the President has:
- Expanded health insurance through the ACA Marketplaces to an additional nine million Americans and helped over one million people in Missouri, North Carolina, Oklahoma, and South Dakota gain Medicaid coverage.
- Extended postpartum Medicaid coverage to nearly 700,000 women across 44 states and the District of Columbia.
- Kept children covered continuously in Medicaid and CHIP for a full year.
- Made it easier for people to enroll in the ACA Marketplaces and Medicaid, including for older adults that are covered by both Medicaid and Medicare.
- Made critical vaccines free for all Medicare beneficiaries as well as adults enrolled in Medicaid, with seniors on Medicare saving on average $70 in out-of-pockets for vaccines.
- Lowered maximum out of pocket costs for Americans with employer and ACA coverage by an average of $400.
- Capped out-of-pocket costs at $35 for a month’s supply of insulin for seniors and people with disabilities on Medicare.
Lowered coinsurance for seniors that took the 47 drugs covered by Medicare Part B that hiked prices faster than inflation in 2023, with some enrollees saving as much as $618 per dose.