By Karen Rubin, [email protected], news-photos-features.com
It boils down to this: Trump/Musk/DOGE are basically stealing the tax money that New Yorkers send to Washington which the federal government is obligated to send back to pay the Social Security, Medicare, Medicaid benefits and other social services that are cumulatively funded by the federal government. And they are stealing that money from the most vulnerable people – the elderly, the disabled, children, veterans, the sick and the poor – in order to further enrich the richest in society.
Out of New York’s $292 billion budget, 40% – $92 billion – is supposed to come back to the states from the federal taxes we pay. Indeed, a “donor state”, New Yorkers pay more into the federal coffers than come back to us, while Red States like Louisiana, Mississippi and Alaska that boast of their low taxes, get way more in federal funding than they pay in income taxes.
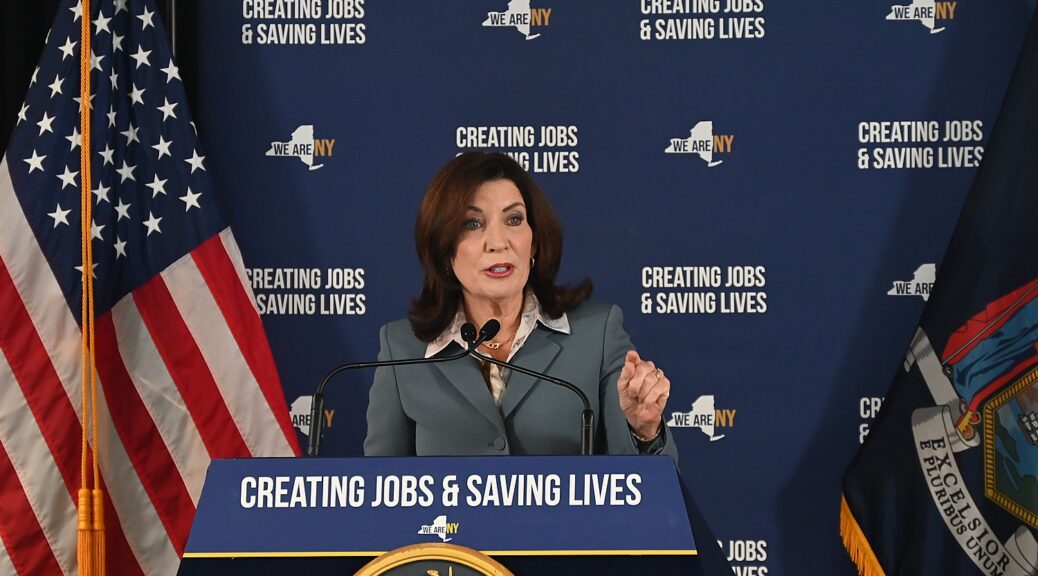
What’s worse is the random, casual, careless way the cuts are being made. “He throws spaghetti to the wall, and what falls down is what’s cut,” Governor Kathy Hochul said at a press conference with US Senator Kirsten Gillibrand to focus attention on the damage being caused to Social Security.
“The Trump administration and DOGE boys are crippling phone support even though appointments can only be made by phone; they plan to cut 7000 staff even though staff numbers are already at a 50 year low; they cut 47 Social Security locations including two in New York State. Meanwhile, 10,000 each day turn 65, all entitled to their earned benefits,” declared U.S. Senator Kirstin Gillibrand.
The cuts in service and the ability to access benefits could be catastrophic, Gillibrand said, “for seniors, people with disabilities who rely on social security to pay for rent, food, heating, medical care – everything they need to survive.” Social security is this nation’s largest anti-poverty program, and arguably its most popular government program.
But it also directly impacts their family and has rippling effect on the economic wellbeing of their community and the state.
“Imagine the impact on New York’s economy if they can’t buy essentials, can’t afford healthcare. It puts greater burden on hospitals, clinics…That doesn’t just affect them, but the community, businesses, services, the entire economy.”
Over 4 million New Yorkers receive Social Security, of which 125,000 are children/ In Albany, alone, 70,000 receive social security. It amounts to $128 million.
Damage has already been done, Gillibrand said. Phone services already in disarray, there is chaos and fear, especially for people unable to travel in person.
“Many of these changes are so severe, more drastic, more radically harmful than ever imagined, I don’t think people fully comprehend. It’s deeply destabilizing. As harm continues to affect every citizen, people will start calling their representative and make them understand their adherence and loyalty to one man is at odds with their constituents, hopefully will then stop,” Senator Gillibrand said.
“We as a society decided government would provide a safety net. If we go back to that time when safety nets don’t exist, more will die in poverty.
“The good news is we have a strong state government strong, but the state budget is affected. We pay so much in federal tax dollars, we expect them to come back to the state. If our federal dollars don’t come back, that means chunks are taken from health care, social security administration, disability. We have to rise up, to convince the seven Republicans to change their mind, to convince Republican senators to stop standing by Trump,” Gillibrand said.

The state was in the final stages of adopting its budget when Trump slashed spending that was already factored in, and there is no way the state can make up for the hole being dug by rescission of federal funds.
“This man [Elon Musk] has enormous power for an unelected official, and he is using it to destroy the very fabric of our safety nets — programs like Social Security,” declared Governor Hochul. “So, he has caused so much chaos and uncertainty. Just walk into this federal building — you can feel it, it’s palpable; the anxiety that the workers here who dedicate their lives to public service, not just here, but all across this country, are under siege. Why? Because they’re out there helping the people.
“That is the whole premise behind becoming a public servant, and those who work for Social Security know that there’s people who rely on them and not everybody knows how to go online and figure it out…..When phone calls aren’t answered, when offices are closed — the offices that have been closed in New York State already — that requires seniors who may not have easy access to get around to go from their community and travel across five to seven different counties. How are they going to get there if they need services in person?
“In New York, our priorities are different,” Governor Hochul said. “We think it’s wrong to say seniors and people with disabilities have to travel a great distance to secure their benefits. We say it’s wrong to describe Social Security as a ‘Ponzi scheme,’ and we say it’s wrong to jeopardize a safety net that has been there to make sure that our citizens never slip into poverty.”
What’s to be done?
Governor Hochul urged constituents to pressure New York State’s seven Republican Members of Congress.
“They are your Republican members of Congress. They’re in the majority, they have the power. If seven members of the delegation from New York State — starting with Elise Stefanik all the way on down — go into the Speaker’s office, demand that there would be changes or you’ll hold up President Trump’s agenda. You have the power, and if you don’t use that power, then you are complicit in this attack on the American people. And so, citizens, residents, people who represent all of our elected officials here: Make sure our voices are heard, make sure our senior’s voices are heard and we have to stop the insanity of this attack on our people.”
Harm to State’s Health Programs
Governor Kathy Hochul also shared a breakdown of the Trump administration’s sweeping federal cuts to New York State’s health programs, and how these cuts to health funding will affect New Yorkers. The amount of funding lost will have a devastating impact statewide on programs that ensure the safety and well-being of people in New York, gutting over $360 million in financial resources toward mental health and addiction services, and health departments across the State.
“Slashing funding for public health, suicide prevention and addiction services is just plain cruel, and it’s going to hurt everyday New Yorkers most,” Governor Hochul said. “Here’s the sad truth: there is no State in the nation that has the resources to backfill these sweeping cuts. It’s up to New York’s elected officials who serve in the House majority to stand up and fight back.”
Federal Cuts by the Numbers:
Department of Health: DOH expects to lose over $300 million in funding for organizations across the State.
- This funding supports many activities that are core to public health functioning, including virus surveillance, outbreak response, electronic data exchange, public dashboards, infection prevention activities in hospitals and nursing homes, laboratory reporting, program operations, and support to local health departments. The backbone of the State’s public health infrastructure will be weakened significantly due to reduced virus surveillance and reporting systems that can no longer provide communities and families with real-time information on developing outbreaks, laboratory support and testing, data collection and analysis, public-facing dashboards, data and analytics.
- Losing this funding will shutter multiple areas of work that are largely seen as foundational components of the Department’s response to emerging infectious diseases. These cuts will also eliminate the Centers for Disease Control (CDC) and Prevention’s COVID-19 Health Disparities Grant, which funded 135 subcontractors to support community-based work addressing health disparities in New York, such as mental health, maternal and infant health, and food security.
Office of Addiction Services and Supports: OASAS expects to lose $40 million total in funding, which will result in significant cuts to addiction and prevention services, treatment supports and access to resources for individuals struggling with substance use. This work includes, but is not limited to:
- Transitional housing to help provide short-term housing and case management for individuals leaving OASAS residential treatment or correctional facilities who cannot otherwise access permanent housing.
- Support for programs, access to treatment, recovery, and other basic services that keep people connected to care in their communities.
- Expansion of outpatient clinics to offer medication for addiction treatment and to purchase and outfit mobile medication units to bring services where they are needed.
- Administering and implementing Screening, Brief Intervention, and Referral to Treatment (SBIRT) which is a comprehensive public health approach to identify those at risk of developing substance use disorders and deliver early intervention and treatment services to individuals who exhibit habits of risky use of alcohol and other substances.
Office of Mental Health: OMH expects to lose $27 million total in funding for programs and services for individuals experiencing mental health and/or substance use needs. These programs were intended to allow individuals in need of care to remain in their homes, connected to their natural support systems during treatment. The loss of this funding will result in an increased reliance on emergency services and hospital-based care with fewer community resources and supports for our most vulnerable New Yorkers, including:
- Crisis Stabilization and Crisis Residence Programs to provide urgent treatment to individuals experiencing an acute mental health and/or substance use crisis, and a safe place for the stabilization of psychiatric symptoms and support for children and adults.
- Adult Assertive Community Treatment Teams (ACT) serving individuals with serious mental illness who are in danger of losing their housing/becoming homeless, are homeless, and/or have histories of involvement with the criminal justice system, and Children and Youth Assertive Community Treatment Teams (ACT) for youth who are returning home from inpatient settings or residential services, at risk of entering such settings, or have not adequately engaged or responded to treatment in more traditional community-based services.
- Grants to expand and improve upon the mobile crisis services statewide, including 9-8-8 crisis call centers. These call centers have relied on this funding to ensure they have capacity to connect callers experiencing emotional distress to the compassionate care of trained counselors.
New York State Department of Health Commissioner Dr. James McDonald said, “It is disappointing these grants were terminated so impulsively without any advance notice and without consideration for the people we serve. We were poorly prepared as a nation for the last pandemic. I see the same pattern occurring now, where decisions are made without consideration for the public’s health and well-being. These grants were preparing us to be healthier for the next pandemic. These investments allowed New York to develop strategies that prevent chronic disease, improve nutrition and find problems before they started.”
“These sweeping federal cuts to health and human services threaten critical addiction funding streams that support prevention, harm reduction, treatment, and recovery services, putting lives at risk and straining the providers working tirelessly on the frontlines of this public health crisis,” Office of Addiction Services and Supports Commissioner Dr. Chinazo Cunningham said. “OASAS remains committed to protecting and expanding access to life-saving services, and will work to mitigate the damage caused by these harmful cuts.”
Office of Mental Health Commissioner Dr. Ann Sullivan said, “For many years, the federal government has been a trusted and valued partner in efforts to provide critical mental health services and supports to New Yorkers, many living in traditionally marginalized communities and under difficult socioeconomic conditions. These drastic cuts will likely slow, and in some instances, halt the fantastic progress our federally funded programs have made and continue to make across our state. We have come too far to reverse course on mental health, which is why our federal legislators owe it to New York to challenge these cuts however possible.”
______________________________
© 2025 News & Photo Features Syndicate, a division of Workstyles,Inc. All rights reserved. For editorial feature and photo information, go to www.news-photos-features.com,email [email protected].Blogging at www.dailykos.com/blogs/NewsPhotosFeatures